Substance use disorders (SUDs) correspond to a range of chronic health conditions defined in the DSM-V as the “recurrent use of alcohol and/or other drugs that causes clinically and functionally significant impairment, such as health problems, disability and failure to meet major responsibilities at work, school, or home” (American Psychiatric Association, 2013). With over 20 million people aged 12 or older in the US that had a SUD related to their use of alcohol or illicit drugs in 2019, substance abuse is a significant public health issue in the US (SAMHSA, 2020). But should SUDs simply be considered as criminal behaviours? Alternatively, are we all at risk of suffering from a SUD at some point in our life? Many scientists argue that SUDs are the result of a pyramid of risk factors that include heredity (i.e., inherited or genetic factors), environment (i.e., environmental and social stressors), and the recurrent use of psychoactive substances (SAMHSA, 2019). Let us examine how heredity and the environment can lead to SUDs.
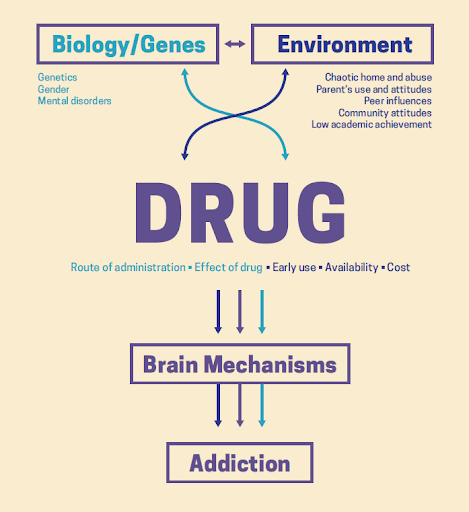
Source: Image copied from NIDA, 2020
Heredity is one of the main risk factors for developing a SUD or another addictive disorder like gambling, and researchers have now identified several genes that are likely to increase the risk of addiction (Deak & Johnson, 2021). The National Institute on Drug Abuse (NIDA) declared that around 50% of someone’s likelihood to develop an addiction, including SUDs, is based on their genes (National Institute on Drug Abuse, 2019). Genetics is something that none of us has control over, and genetic predispositions could put any individual at risk of developing a SUD in their life.
However, having a genetic predisposition to SUDs does not necessarily mean that one will actually suffer from a SUD. A person’s health results from interactions between their genes and their environment. Some environmental factors such as an individual’s socio-economic level, access the healthcare, access to substances (illicit drugs or prescription medications), levels of exposure to stress, and the behaviors of people in their social network are known risk factors of SUDs (Mennis et al., 2016; SAMHSA, 2019).
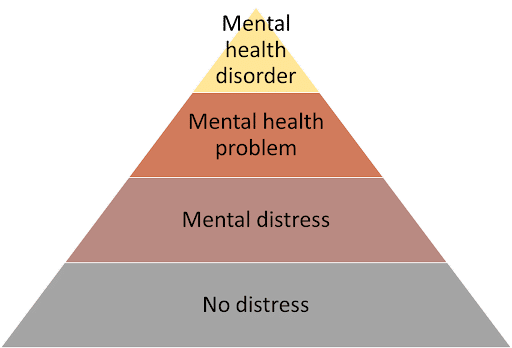
Stress refers to an individual’s perception and response to harmful or challenging life events. When an individual faces a stressful situation, their brain activates physiological stress responses and adaptive processes to regain homeostasis (Ewald et al., 2019). However, an individual’s ability to cope with stressful events depends on the type of stimulus that triggered distress. This corresponds to the “distress” pyramid, which illustrates how an individual can progress between four states: 1) no distress (the individual is doing fine), 2) mental distress (refers to everyday life problems, usually easily overcome by individuals), 3) mental health problems (severe events in an individual’s life such as a divorce or the death of a close relative, which may cause intense stress and emotions), and 4) mental health disorders (medically diagnosed psychiatric conditions) (Kutcher, 2021).
Research shows that early exposure to adverse life events such as the loss of a close relative, parental divorce, domestic violence, and sexual abuse is associated with an increased risk of substance abuse (Forster et al., 2018). Exposure to these significant environmental stressors can change the brain’s neuroendocrine hypothalamic-pituitary-adrenal axis with significant conditioning effects on decision-making functions and behaviors. These changes play an essential role in the initiation of substance use and the risk of progression from substance use to SUD (Ewald et al., 2019; SAMHSA, 2019).
Likewise, chronic exposure to distress in an individual’s personal life or workplace can also influence their brain’s response to stressful events and predict their vulnerability to SUDs (Ewald et al., 2019). There is considerable evidence supporting the role of psychosocial adversity, negative affect, and chronic distress in enhancing the susceptibility to substance use and abuse, the progress from substance use to SUDs, and the risk of relapses (Sinha, 2008; Torres-Berrio et al., 2018). Previous research suggests that cumulative adversity (the cumulative number of stressful events experienced in one’s life) is significantly predictive of substance abuse with a dose-dependent relationship, even after accounting for important control factors such as gender, ethnicity, history of substance use, or socioeconomic status (Mukhara et al., 2018; Sinha, 2008). The more prolonged or repeated the exposure to distress, the higher the risk for persistent dysregulation of an individual’s mental health and the higher the risk of developing SUDs.
In other words, combining high levels of stress or chronic exposure to stress with easy access to substances is the perfect incubator for SUDs. This has a significant implication. Contrary to common belief, many people suffering from SUDs are not “criminals” or “marginalized people”. On the contrary, there are many people who, because of unmanageable stress levels in their personal life or in their workplace, start misusing prescription medication or using illicit drugs as a coping mechanism and progress to a SUD. The key take-home message is that anyone is at risk of suffering from SUDs in their life, especially when exposed to high levels of distress or frequent adverse events.

Because everyone is at risk, community-based interventions are particularly well suited to address SUDs. Interventions that take place in the community can help prevent SUDs and contribute to the treatment of SUDs (Surgeon General, 2016). According to the United Nations Office for Drugs and Crimes, community-based treatment is the most cost-effective SUD treatment approach (UNODC, 2014).
Community-based treatment can facilitate patients’ access to treatment, are usually more affordable for patients and their families, can foster patients’ independence in their natural environment, are less intrusive and less disruptive to daily life as compared to other modalities of treatment, and facilitate the reduction of stigma related to SUDs (UNODC, 2014).
As previously mentioned, distress progression is one of the main risk factors for SUDs. How can community-based interventions help protect people from the negative consequences associated with chronic distress? Brief interventions aimed at improving an individual’s level of distress tolerance, i.e., “one’s ability to continue engaging in goal-directed behaviour in the face of emotional, cognitive, or physical discomfort,” can easily be delivered in the community by people who are not mental health or addiction specialists (Castillo et al., 2019; Lotan et al., 2013; Russell et al., 2019; Wright et al., 2020). These interventions on distress tolerance may be helpful both as preventive and treatment levers for SUDs. First, research suggests that greater distress tolerance is associated with a lower risk of developing a SUD but also with better outcomes for SUD treatment, such as increased efficiency of treatment and lower frequency of relapses. On the contrary, lower distress tolerance could be associated with a higher risk of developing SUDs (Bornovalova et al., 2012; Kechter et al., 2021; Reese et al., 2019). Likewise, other stress management and mindfulness brief interventions delivered in the community could help prevent SUDs or be used as part of a therapeutic approach (Chiesa & Serretti, 2014; Nakamura et al., 2015; Reynolds et al., 2020).
To conclude, let us keep this quotation in mind: “No one is immune from addiction; it afflicts people of all ages, races, classes, and professions.”– Patrick J. Kennedy, American politician, and mental health activist.
References
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders: DSM-5TM, 5th ed (pp. xliv, 947). American Psychiatric Publishing, Inc. https://doi.org/10.1176/appi.books.9780890425596
Bornovalova, M. A., Gratz, K. L., Daughters, S. B., Hunt, E. D., & Lejuez, C. W. (2012). Initial RCT of a distress tolerance treatment for individuals with substance use disorders. Drug and Alcohol Dependence, 122(1), 70–76. https://doi.org/10.1016/j.drugalcdep.2011.09.012
Castillo, E. G., Ijadi-Maghsoodi, R., Shadravan, S., Moore, E., Mensah, M. O., Docherty, M., Aguilera Nunez, M. G., Barcelo, N., Goodsmith, N., Halpin, L. E., Morton, I., Mango, J., Montero, A. E., Rahmanian Koushkaki, S., Bromley, E., Chung, B., Jones, F., Gabrielian, S., Gelberg, L., … Wells, K. B. (2019). Community Interventions to Promote Mental Health and Social Equity. Current Psychiatry Reports, 21(5), 35. https://doi.org/10.1007/s11920-019-1017-0
Chiesa, A., & Serretti, A. (2014). Are Mindfulness-Based Interventions Effective for Substance Use Disorders? A Systematic Review of the Evidence. Substance Use & Misuse, 49(5), 492–512. https://doi.org/10.3109/10826084.2013.770027
Deak, J. D., & Johnson, E. C. (2021). Genetics of substance use disorders: A review. Psychological Medicine, 51(13), 2189–2200. https://doi.org/10.1017/S0033291721000969
Ewald, D. R., Strack, R. W., & Orsini, M. M. (2019). Rethinking Addiction. Global Pediatric Health, 6, 2333794X18821943. https://doi.org/10.1177/2333794X18821943
Forster, G. L., Anderson, E. M., Scholl, J. L., Lukkes, J. L., & Watt, M. J. (2018). Negative consequences of early-life adversity on substance use as mediated by corticotropin-releasing factor modulation of serotonin activity. Neurobiology of Stress, 9, 29–39. https://doi.org/10.1016/j.ynstr.2018.08.001
Kechter, A., Barrington-Trimis, J. L., Cho, J., Davis, J. P., Huh, J., Black, D. S., & Leventhal, A. M. (2021). Distress tolerance and subsequent substance use throughout high school. Addictive Behaviors, 120, 106983. https://doi.org/10.1016/j.addbeh.2021.106983
Kutcher, S. (2021). Mental Health. We Mind & Kelly Matters. https://wemindandkellymatters.org.uk/help-advice/mental-health/
Lotan, G., Tanay, G., & Bernstein, A. (2013). Mindfulness and Distress Tolerance: Relations in a Mindfulness Preventive Intervention. International Journal of Cognitive Therapy, 6(4), 371–385. https://doi.org/10.1521/ijct.2013.6.4.371
Mennis, J., Stahler, G. J., & Mason, M. J. (2016). Risky Substance Use Environments and Addiction: A New Frontier for Environmental Justice Research. International Journal of Environmental Research and Public Health, 13(6), 607. https://doi.org/10.3390/ijerph13060607
Mukhara, D., Banks, M. L., & Neigh, G. N. (2018). Stress as a Risk Factor for Substance Use Disorders: A Mini-Review of Molecular Mediators. Frontiers in Behavioral Neuroscience, 12. https://www.frontiersin.org/article/10.3389/fnbeh.2018.00309
Nakamura, Y., Lipschitz, D. L., Kanarowski, E., McCormick, T., Sutherland, D., & Melow-Murchie, M. (2015). Investigating Impacts of Incorporating an Adjuvant Mind–Body Intervention Method Into Treatment as Usual at a Community-Based Substance Abuse Treatment Facility: A Pilot Randomized Controlled Study. SAGE Open, 5(1), 2158244015572489. https://doi.org/10.1177/2158244015572489
National Institute on Drug Abuse. (2019, August 5). Genetics and Epigenetics of Addiction. National Institute on Drug Abuse. https://nida.nih.gov/publications/drugfacts/genetics-epigenetics-addiction
National Institute on Drug Abuse. (2020). Drugs, Brains, and Behavior: The Science of Addiction. https://nida.nih.gov/publications/drugs-brains-behavior-science-addiction/preface
Reese, E. D., Conway, C. C., Anand, D., Bauer, D. J., & Daughters, S. B. (2019). Distress tolerance trajectories following substance use treatment. Journal of Consulting and Clinical Psychology, 87(7), 645–656. https://doi.org/10.1037/ccp0000403
Reynolds, L., Rogers, O., Benford, A., Ingwaldson, A., Vu, B., Holstege, T., & Alvarado, K. (2020). Virtual Nature as an Intervention for Reducing Stress and Improving Mood in People with Substance Use Disorder. Journal of Addiction, 2020, 1892390. https://doi.org/10.1155/2020/1892390
Russell, B. S., Lincoln, C. R., & Starkweather, A. R. (2019). Distress Tolerance Intervention for Improving Self-Management of Chronic Conditions: A Systematic Review. Journal of Holistic Nursing, 37(1), 74–86. https://doi.org/10.1177/0898010118777327
SAMHSA. (2019). Risk and Protective Factors. Substance Abuse and Mental Health Services Administration. https://www.samhsa.gov/sites/default/files/20190718-samhsa-risk-protective-factors.pdf
SAMHSA. (2020). Key Substance Use and Mental Health Indicators in the United States: Results from the 2019 National Survey on Drug Use and Health. Substance Abuse and Mental Health Services Administration. https://store.samhsa.gov/product/key-substance-use-and-mental-health-indicators-in-the-united-states-results-from-the-2019-national-survey-on-Drug-Use-and-Health/PEP20-07-01-001
Sinha, R. (2008). Chronic Stress, Drug Use, and Vulnerability to Addiction. Annals of the New York Academy of Sciences, 1141, 105–130. https://doi.org/10.1196/annals.1441.030
Surgeon General. (2016). Early Intervention, Treatment, and Management of Substance Use Disorders | Surgeon General’s Report on Alcohol, Drugs, and Health. Surgeon General. https://addiction.surgeongeneral.gov/executive-summary/report/early-intervention-treatment-and-management-substance-use-disorders
Torres-Berrio, A., Cuesta, S., Lopez-Guzman, S., & Nava-Mesa, M. O. (2018). Interaction Between Stress and Addiction: Contributions From Latin-American Neuroscience. Frontiers in Psychology, 9. https://www.frontiersin.org/article/10.3389/fpsyg.2018.02639
UNODC. (2014). Community Based Treatment and Care for Drug Use and Dependence—Information Brief for Southeast Asia. United Nations Office for Drugs and Crimes. https://www.unodc.org/documents/southeastasiaandpacific/cbtx/cbtx_brief_EN.pdf
Wright, I., Travers-Hill, E., Gracey, F., Troup, J., Parkin, K., Casey, S., & Kim, Y. (2020). Brief psychological intervention for distress tolerance in an adult secondary care community mental health service: An evaluation. The Cognitive Behaviour Therapist, 13. https://doi.org/10.1017/S1754470X20000513
